ESC 2022 Highlights
The latest in Acute Coronary Syndrome from ESC 2022
From the 2022 European Society of Cardiology (ESC) congress in Barcelona, receive original content on developments in acute coronary syndrome (ACS) treatments, focusing on international guideline updates, and antiplatelet therapies such as P2Y12 inhibitors.
Interview with Professor Magdy Abdelhamid
Overview of Acute Coronary Syndrome: Signs, pathophysiology, and epidemiology
In this short video clip, Professor Magdy Abdelhamid (Cardiology Department at the Faculty of Medicine, Cairo University, Egypt) summarises the common signs and markers of pathophysiology of ACS. He also surveys prevalence and incidence data on ACS.
Guideline recommendations for anti-platelet therapy for ACS
Professor Abdelhamid reviews criteria for the use of antiplatelet therapy for people with ACS, including beyond the recommended twelve months. Risk of bleeding, he emphasises, should be assessed using a variety of clinical measures, and is higher in people above the age of 65, people with diabetes, among other factors. Watch the video to learn more.
Anti-platelet therapy options for Acute Coronary Syndrome
Watch the video below to learn options for anti-platelet therapy for ACS. Professor Abdelhamid reviews the use of newer options for patients, such as aspirin and P2Y12 inhibitors, and extended dual antiplatelet therapy (DAPT) for people with ACS at high-risk of ischaemic events. He summarises treatment goals for ACS.
*300 milligram1.
New clinical trial data for ACS and anti-platelet therapy, presented at ESC 2022
ESC 2022 was an opportunity for investigators to present recent clinical trial data on anti-platelet efficacy and safety for ACS. In this video summary, Professor Abdelhamid highlights some of these important findings.
Meet the expert
 Professor Magdy Abdelhamid
Professor Magdy Abdelhamid
Magdy Abdelhamid is a Professor and Chairman of the Cardiology Department at the Faculty of Medicine, Kasr El Ainy, Cairo University, Egypt. He is a consultant cardiologist with more than 30 years of clinical experience, and has a particular interest in heart failure and coronary intervention. Professor Abdelhamid is the Past President of the Egyptian Society of Cardiology (2018–2020), and Chairman of their working group on heart failure, and a Board member of the Society. He is a Board Member of the Heart Failure Association of the ESC (2020-2022), Co-Chair of the Acute Heart Failure Scientific Committee of HFA, ESC (2020–2022), and Co-Chair of the Valvular Heart Disease Scientific Committee of HFA, ESC (2020–2022). Professor Abdelhamid is a member of the Committee of Practice Guidelines, ESC (2020–2022). Currently, Professor Abdelhamid is nominated as Co-Chair of the Educational Committee of the HFA, ESC (2022–2024), and Board member of the Educational Committee of the ESC (2022–2024).
Professor Abdelhamid is a Fellow of the American College of Cardiology (FACC), The European Society of Cardiology (FESC), the Royal College of Physicians and Surgeons (FRCP) of Glasgow, European Heart Failure Association (FHFA), and the Society for Cardiovascular Angiography and Interventions (FSCAI).
Disclosures
Professor Abdelhamid has no disclosures to report.
Reference
- Fox KAA, Mehta SR, Peters R, Zhao F, Lakkis N, Gersh BJ, et al. Benefits and Risks of the Combination of Clopidogrel and Aspirin in Patients Undergoing Surgical Revascularization for Non–ST-Elevation Acute Coronary Syndrome. Circulation. 2004;110(10):1202–1208.
Identifying the optimal timing for P2Y12 inhibitor pre-treatment in patients with STEMI
Dr João Presume presented the results of a meta-analysis of studies on dual antiplatelet therapy (DAPT) with aspirin and P2Y12 inhibitors, highlighting the importance of antithrombotic therapy in patients with ST-segment elevation myocardial infarction (STEMI)1. However, there is still uncertainty surrounding the optimal timing for initiating P2Y12 inhibitor therapy2. The aim of the meta-analysis was to elucidate the effectiveness and safety of P2Y12 pre-treatment.
A systematic search of electronic databases was conducted for studies that compared P2Y12 inhibitor pre-treatment with treatment during primary percutaneous coronary intervention (PCI), and in which patients were enrolled for STEMI and submitted to primary PCI. Major clinical outcomes analysed included definite stent thrombosis, re-infarction and all-cause death. Other events analysed included in-hospital cardiogenic shock, and thrombolysis in myocardial infarction (TIMI) flow grade pre-PCI and post-PCI.
Pre-treatment with P2Y12 inhibitors was associated with a lower risk of definite stent thrombosis and cardiogenic shock, but not with a lower re-infarction or all-cause death rate
Of 2193 studies identified by the search, 18 were included in the meta-analysis, with a total of 76,836 patients, of whom 52,181 were in the pre-treatment arm. At the 30-day mark, there was an association with pre-treatment and a reduction in definite stent thrombosis (one randomised controlled trial [RCT] and four on-RCT: odds ratio [OR] 0.40; 95% confidence intervals [CI] 0.18–0.90), but no significant reduction in all-cause death (one RCT and seven non-RCT: OR 0.77; 95% CI 0.56–1.04)or re- infarction (one RCT and four non-RCT: OR 0.73; 95% CI 0.49–1.09).
The results showed a significant reduction in the occurrence of in-hospital cardiogenic shock in patients who received P2Y12 inhibitor pre-treatment (five non-RCT: 0.62; 95% CI 0.51–0.79), the number of patients with TIMI flow <3 post-PCI (one RCT and eight non-RCT: 0.82; 95% CI 0.73–0.93) and in major bleeding events (one RCT and 14 non-RCT: 0.83; 95% CI 0.75–0.92).
Dr Presume concluded that pre-treatment with DAPT, including a P2Y12 inhibitor, had no association with a lower re-infarction or all-cause death rate but was associated with a reduced risk of definite stent thrombosis and cardiogenic shock.
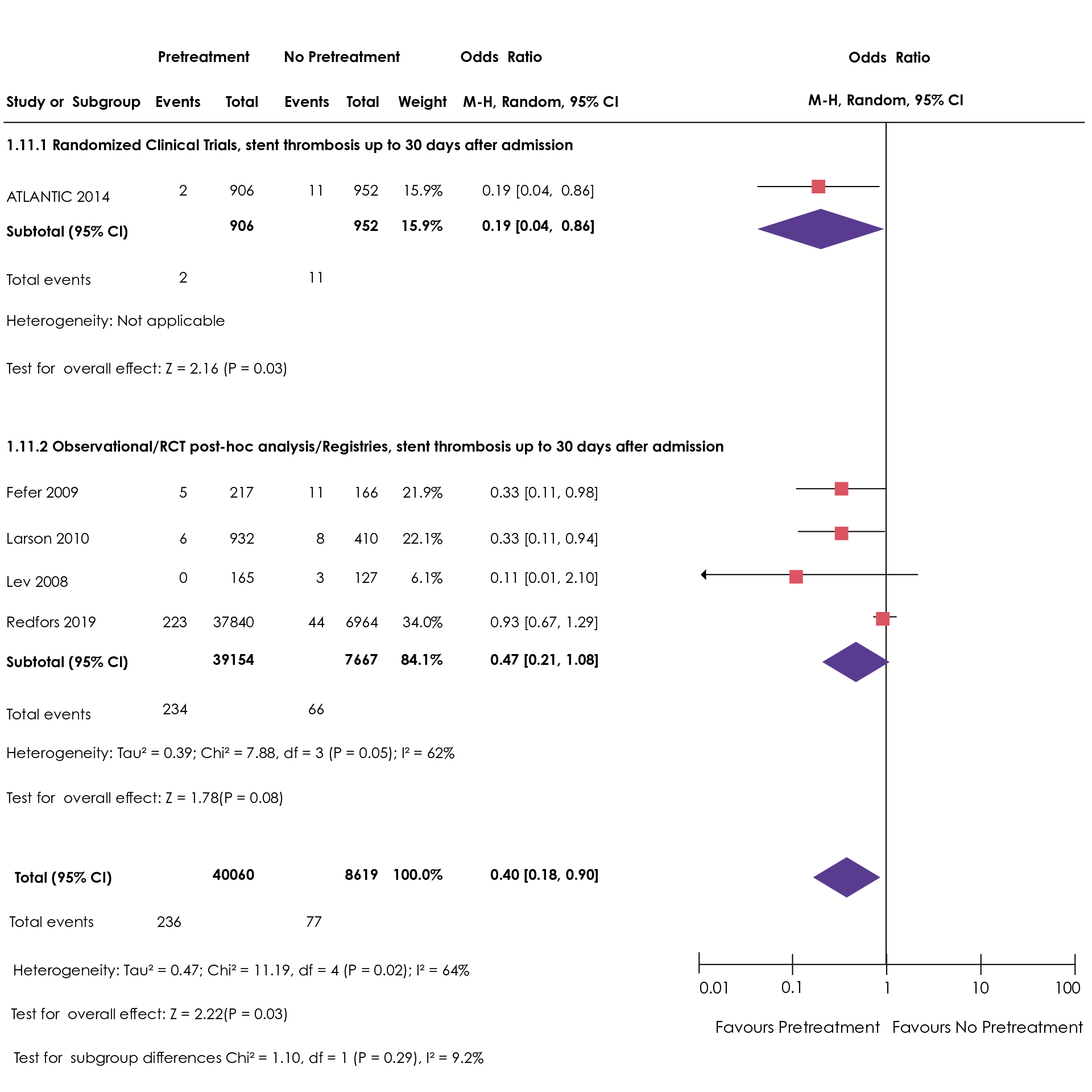
Figure 1. Treatment and pre-treatments odd ratios for the randomised ATLANTIC 2014 study1 (CI, confidence interval; RCT, randomised clinical trial).
The comparative efficacy and safety of ticagrelor versus prasugrel in ACS
Over time, the standard treatment for patients with the non-ST segment elevation acute coronary syndrome (NSTE-ACS) has come to consist of dual antiplatelet therapy (DAPT), consisting of a P2Y12 inhibitor and aspirin3, with current guidelines recommending prasugrel and ticagrelor over clopidogrel4. The ISAR-REACT 5 clinical trial showed that in NSTE-ACS patients, prasugrel was superior to ticagrelor5; however, Professor Uwe Zeymer and colleagues analysed real-world data to evaluate the outcomes of patients undergoing primary percutaneous coronary intervention (PCI) for NSTE-ACS being treated with either prasugrel or ticagrelor6.
The study collected data from the German ALKK-PCI registry and included patients from 42 centres who were treated with ticagrelor or prasugrel. Antithrombotic therapies, in-hospital shock, baseline variable and procedural features were analysed, but patients with cardiogenic shock were excluded from the study.
Professor Zeymer presented the results of the investigation. In the nine years between 2011 and 2020, a total of 7888 patients aged <75 years without prior history of undergoing PCI for NSTE-ACS were included in the study, with 4905 patients being treated with ticagrelor (62.2%) and 2983 patients being treated with prasugrel (37.8%).
The study concluded that ticagrelor was used more often than prasugrel in patients with NSTE-ACS undergoing PCI. Patients treated with ticagrelor were older and had more comorbidities than those treated with prasugrel. Despite the higher risk associated with the ticagrelor group, there was a similar short-term safety profile for both drugs regarding in-hospital mortality rates, bleeding and non-fatal strokes.
Evaluation of temporal trends in the treatment and outcomes of ACS patients according to bleeding risk
Adverse clinical outcomes in patients with acute coronary syndrome (ACS) have been shown to correlate with high bleeding risk7. Dr Ziad Arow presented the findings of a study that aimed to explicate this trend by evaluating the treatment trends in the treatment and outcomes of ACS patients according to bleeding risk8.
Overall, patients with a high bleeding risk were more susceptible to 30-day MACE and 1-year all-cause mortality
For their study, Dr Arow and colleagues included patients with ACS who were enrolled in the ACSIS survey and categorised their bleeding risk according to the CRUSADE score. The patients were initially split into three chronologically stratified groups, early (2002–2004), mid (2006–2010) and recent (2012–2018), according to enrolment period. These groups were then split into three sub-groups, low, medium and high, according to their bleeding risk. The research group used 30-day major adverse cardiovascular events (MACE) and 1-year all-cause mortality as end-points.
Following the enrolment of individuals from the ACSIS survey, 13,058 ACS patients were included in the study. It was first shown that overall, patients with a high bleeding risk were more susceptible to 30-day MACE and 1-year all-cause mortality in all groups across all three enrolment periods (early, mid and recent). The data collected by Dr Arow and colleagues were divided into two sets of results: the 30-day MACE rates, followed by 1-year all-cause mortality rates.
The 30-day MACE rates were 10.8%, 17.5% and 24.3% for patients enrolled in the early period, 7.7%, 13.4%, and 23.5% for those enrolled during the mid-period, and 5.7%, 8.6% and 16.2% for those enrolled during the recent period in low, moderate, and high bleeding risk groups, respectively.
Additionally, the 1-year all-cause mortality rates were 2%, 7.7% and 23.6% (P<0.001) in those enrolled during the early period, 1.5%, 7.2% and 22.1% (P<0.001) enrolled during the mid-period, and for patients enrolled in the recent period, 1-year all-cause mortality rates were 2.1%, 6% and 22.4%, (P<0.001) in the low, moderate and high bleeding risk groups, respectively.
Dr Arow concluded that despite significant advancements in the treatment of ACS patients, clinical outcomes are strongly correlated with high bleeding risk.
References
- Presume J. 30-day outcomes of P2Y12 inhibitor pre-treatment in patients with STEMI submitted to primary PCI – systematic review and meta-analysis. Presented at the European Society of Cardiology Congress 2022, 27 August. Barcelona. Moderated ePosters. Antithrombotic and anticoagulant therapy.
- Araiza-Garaygordobil D, Gopar-Nieto R, Sierra-Lara Martínez D, et al. Dual antiplatelet therapy versus antiplatelet monotherapy plus oral anticoagulation in patients with acute coronary syndrome and coronary artery ectasia: design and rationale of OVER-TIME randomized clinical trial. High Blood Press Cardiovasc Prev. doi:10.1007/s40292-022-00535-4
- Barbato E, Mehilli J, Sibbing D, et al. Questions and answers on antithrombotic therapy and revascularization strategies in non-ST-elevation acute coronary syndrome (NSTE-ACS): a companion document of the 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2020;42(14):1368–1378. doi:10.1093/eurheartj/ehaa601
- Adamski P, Barańska M, Ostrowska M, et al. Diurnal variability of platelet aggregation in patients with myocardial infarction treated with prasugrel and ticagrelor. J Clin Med. 2022;11(4):1124. doi:10.3390/jcm11041124
- Schüpke S, Neumann FJ, Menichelli M, et al. Ticagrelor or Prasugrel in Patients with Acute Coronary Syndromes. New England Journal of Medicine. 2019;381(16):1524-1534. doi:10.1056/nejmoa1908973
- Zeymer U, Hochadel M, Schaechinger V, Zahn R. Comparative efficacy and safety of ticagrelor versus prasugrel in patients undergoing PCI for NSTE-ACS. Results of the prospective ALKK-Registry. Presented at the European Society of Cardiology Congress 2022, 28 August. Barcelona. Platelets and More. Moderated ePosters.
- Han K, Shi D, Yang L, et al. Prognostic value of systemic inflammatory response index in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Ann Medi. 2022;54(1):1667-1677. doi:10.1080/07853890.2022.2083671
- Arow Z. Temporal trends in the treatment and outcomes of patients with acute coronary syndrome according to bleeding risk. Presented at the European Society of Cardiology Congress 2022, 28 August. Barcelona. Acute Coronary Syndromes – Risks. Moderated ePosters.
The obesity paradox in patients with acute coronary syndromes
It is well acknowledged that obesity is a major epidemic linked to significant risk factors associated with cardiovascular disease (CVD)1. Despite this, a substantial body of data, primarily published over a decade ago, has demonstrated an obesity paradox2, which implies that patients who are obese have better long-term and short-term prognoses than their leaner counterparts with the same CVD profile. Previous research examining the obesity paradox in acute coronary syndrome (ACS) showed that body mass index (BMI) and mortality associations follow a U-shaped curve: patients who are either underweight (BMI <19 kg/m2) or severely obese (BMI >44 kg/m2) have the highest mortality rates, and those who are overweight or mildly obese (BMI 30–34 kg/m2 and BMI 35–39 kg/m2 respectively) have the lowest rates3,4.
Dr Chen Gurevitz and colleagues aimed to elucidate whether this purported obesity paradox in patients with ACS is still relevant in the current era by examining temporal trends in the clinical outcomes of ACS patients by their BMI status. The research group approached this study by deriving statistical data from the ACSIS registry, including all patients with calculated BMIs enrolled between 2000 and 2018. Patients were grouped according to their BMI (underweight, normal, overweight and obese). Clinical endpoints were 30-day major adverse cardiovascular events (MACE) and 1-year mortality. A comparison of trends between the late period (2010–2018) and the early period (2000–2008) was conducted, and a multivariate model was used to examine factors associated with clinical outcomes according to BMI. Dr Gurevitz presented the findings of the study at the ESC 2022 Congress5.
Studies show that patients with ACS who are overweight or obese experience lower 30-day MACE and 1-year mortality than those who are underweight or normal weight
The ACSIS registry contains 13,816 patients with BMI information. Of these patients, 104 were underweight, 3921 were normal weight, 6224 were overweight and 3567 were obese. The investigation revealed that underweight patients had the highest mortality rate (24.8%) than those in the normal weight range (10.7%). Interestingly, patients who were overweight or obese had the lowest mortality rates (7.1% and 7.5%, respectively; P for trend 0.001).
Dr Gurevitz reported a similar pattern for MACE as seen with mortality rates: MACE rates at 30 days were highest in the underweight group (24%), followed by normal weight (13.6%), and lowest in the overweight and obese groups (11.6% and 11.7% respectively; P for trend < 0.001). All BMI groups, excluding the underweight group, had significantly lower 30-day MACE in the late period when comparing the two time periods. It is also noteworthy that the 1-year mortality rate for those in the underweight group had not changed over the two period, while the rate for those in the other three groups declined. The results of this study indicate that patients with ACS are still susceptible to the obesity paradox in the present day.
The association between DAPT score and long-term mortality post PCI
Dr Mae Chyi Tan and colleagues sought to examine long-term mortality after percutaneous coronary intervention (PCI) by the dual antiplatelet therapy (DAPT) score in patients treated with DAPT according to local guidelines6. The score was developed as a way to predict which patients are most likely to benefit (≥2) and those likely to be harmed (<2) by DAPT for more than 1 year after PCI7. In her presentation at ESC 2022, Dr Tan highlighted that no other studies have examined the relationship between the DAPT score and long-term outcomes following PCI in Australia.
The group conducted an analysis of data for patients listed in the Melbourne Interventional Group (MIG) PCI database from 2005–2018 in whom DAPT scores could be determined. Scores were grouped into ≥2 or <2. A long-term mortality analysis was conducted using the National Death Index linkage, in which a survival analysis was used to examine long-term mortality. The primary endpoint of the study was long-term mortality over time. The study's secondary endpoints included 30-day ischaemic outcomes and significant bleeding during hospitalisation.
A total of 27,740 patients were included in the study and of those, 9,401 (33.9%) had a DAPT score ≥2. Dr Tan acknowledged that patients in this group were younger and had a higher prevalence of renal impairment. There were also more females in this group. Patients with DAPT scores ≥2 were shown to be more likely to experience significant bleeding in hospital and myocardial infarction (MI), and more likely to have new target vessel revascularisations and a higher 30-day mortality rate. Dr Tan also reported that patients with a DAPT score of ≥2 had a lower long-term survival rate of 12 years (P<0.001 for all).
According to the study, a third of patients undergoing PCI had a DAPT score of ≥2, which was associated with an increased risk of short-term ischaemic and bleeding events, as well as long-term mortality. It was, however, also theorised that patients with a DAPT score ≥2 would benefit from an extended period of DAPT as the risk of bleeding was outweighed by the reduced risk of ischaemic attacks. The group's findings regarding increased short-term bleeding risk and long-term mortality should guide pharmacotherapy strategies by a dynamic bleeding risk assessment.
Patients with DAPT scores ≥2 were shown to be more likely to experience adverse CV outcomes, including significant in-hospital bleeding and MI, requiring target vessel revascularisations, as well as a higher 30-day mortality rate
Effects of CYP3A4*22 carrier and CYP3A5 expressor status on clinical outcomes in patients treated with ticagrelor
The CYP3A4 enzyme is primarily responsible for the metabolism of ticagrelor, with the CYP3A5 contributing to a lesser extent. The expressor status of the CYP3A variants CYP3A4*22 has been implicated in reduced metabolism of ticagrelor, resulting in increased plasma concentrations and increased platelet inhibition function8. Individuals with CYP3A5 variants, which are thought to increase drug metabolism, are known as CYP3A5 expressors9. However, the impact of the CYP3A4*22 allele or CYP3A5 expressor status on clinical outcomes in ticagrelor-treated patients is not yet fully understood10.
Dr Jaouad Azzahhafi and colleagues aimed to assess how the CYP3A4*22 allele and the CYP3A5 expressor status affect clinical outcomes and dyspnoea in patients with ST-segment elevation myocardial infarction (STEMI) who are treated with ticagrelor11. The group genotyped patients from the POPular Genetics trial for the CYP3A4*22 and CYP3A5*3 alleles12. The patients were split into groups according to their CYP3A4 and CYP3A5 status (CYP3A4*22 carriers or non-carriers, and CYP3A5 expressors or non-expressors). The primary endpoint of the study was a composite of cardiovascular death, myocardial infarction (MI), stroke and definite stent thrombosis. PLATO major and minor bleeding were the primary bleeding outcomes. In this study, dyspnoea was considered one of the most important secondary endpoints and patients were followed up for 1 year.
CYP3A4*22 carriers and CYP3A5 expression in STEMI patients treated with ticagrelor did not correlate with the onset of thrombotic events, bleeding rate or dyspnoea
The analysis presented by Dr Azzahhafi was based on data from 1,281 patients with STEMI. No significant correlation was found for CYP3A4*22 carriers (n = 152) versus non-carriers (n = 1,129) and the primary thrombotic outcome (1.3% versus 2.5%, hazard ratio [HR] 1.81, 95% confidence intervals [CI] 0.43–7.62) or the primary bleeding outcome (13.2% versus 11.3%, HR 0.93, CI 0.58–1.50). In addition, CYP3A5 expressors (n = 196) versus non-expressors (n = 926) did not show a significant difference for the primary thrombotic outcome (2.6% versus 2.5%, HR 1.03, CI 0.39–2.71) or the primary bleeding outcome (12.8% versus 10.9%, HR 1.13, CI 0.73-1.76). Finally, Dr Azzahhafi presented data showing that for dyspnoea, there was no significant difference between CYP3A4*22 carriers and non-carriers (44.0% versus 45.0%, risk ratio 1.04, CI 0.45–2.42) or between CYP3A5 expressors versus CYP3A5 non-expressors (35.3% versus 47.8%, risk ratio 0.60, CI, 0.27–1.30).
Dr Azzahhafi concluded that neither the presence of CYP3A4*22 nor CYP3A5 expression affected bleeding rates, the occurrence of thrombotic events or dyspnoes in patients with STEMI treated with ticagrelor.
References
- Hasebe T, Hasebe N. Impact of risk factors related to metabolic syndrome on acute myocardial infarction in younger patients. Hypertension Research. 2022;45(9):1447-1458. doi:10.1038/s41440-022-00951-y
- Lavie CJ, daSilva‐deAbreu A, Ventura HO, Mehra MR. Is There an Obesity Paradox in Cardiogenic Shock? Journal of the American Heart Association. 2022;11(11). doi:10.1161/jaha.122.026088
- Ahmed F, Abugroun A, Gaznabi S, Klein L. Circulation. 2018;138:A12438.
- Williams MJA, Lee M, Alfadhel M, Kerr AJ. Heart Lung Circ. 2021;30(12):1854-1862.
- Gurevitz C. The obesity paradox in patients with acute coronary syndromes – is it still applicable to the current era? The ACSIS registry 2000-2018. Presented at the European Society of Cardiology Congress 2022, 26 August. Barcelona. Epidemiology, Risks for acute coronary syndrome.
- Tan M. Associations between DAPT score and long-term mortality post PCI. Presented at the European Society of Cardiology Congress 2022, 27 August. Barcelona. Antithrombotic and anticoagulant therapy. Moderated ePosters
- Dannenberg L, Afzal S, Czychy N, et al. Risk prediction of bleeding and MACCE by PRECISE-DAPT score post-PCI. IJC Heart & Vasculature. 2021;33:100750. doi:10.1016/j.ijcha.2021.100750
- Mulder TAM, van Eerden RAG, de With M, et al. Front Genet, 2021;12:711943, doi: 10.3389/fgene.2021.711943
- Brunet M, Pastor-Anglada M. Insights into the Pharmacogenetics of Tacrolimus Pharmacokinetics and Pharmacodynamics. Pharmaceutics. 2022;14(9):1755. doi:10.3390/pharmaceutics14091755
- Liu J, Feng D, Kan X, et al. Pharmacogenomics. 2021;22(14):903-912.
- Azzahhafi J. Effects of CYP3A4*22 carrier and CYP3A5 expressor status on clinical outcome in patients treated with ticagrelor for acute coronary syndrome. Presented at the European Society of Cardiology Congress 2022, 28 August. Barcelona. Coronary Artery Disease – Pharmacotherapy 2. ePosters.
- Claassens DMF, Vos GJA, Bergmeijer TO, et al. A genotype-guided strategy for oral P2Y12 inhibitors in primary PCI. N Engl J Med. 2019;381(17):1621-1631. doi:10.1056/nejmoa1907096
Lipoprotein(a), cardiovascular events, and benefit of P2Y12 inhibition: insights from the PEGASUS-TIMI 54 trial
Given its structural homology with plasminogen but lack of protease activity, lipoprotein(a) [Lp(a)] has been theorised to exert prothrombotic effects by inhibiting fibrinolysis1; as such, it is suggested that antithrombotic therapy may be more beneficial in patients with an above average concentration of Lp(a). Dr Siddharth Patel and colleagues investigated whether patients with elevated Lp(a) levels benefit more from P2Y12 inhibition with ticagrelor versus placebo when aspirin is prescribed2.
As part of PEGASUS-TIMI 54, a randomised trial in which ticagrelor is compared with placebo in patients who had a myocardial infarction (MI) in the previous 3 years3, the Lp(a) concentration was measured in a nested cohort of 8,967 patients and the risk threshold was established at 200 nmol/L. The pre-specified major adverse cardiovascular event (MACE) endpoint was a composite of cardiovascular death, MI or stroke, with Kaplan Meier rates reported at 3 years. Dr Patel's team used Cox proportional hazards to assess the relationship between Lp(a), MACE and the benefits of treatment, and the models were adjusted to consider relevant baseline characteristics, such as the level of apolipoprotein B.
An Lp(a) value exceeding 200 nmol/L is associated with an increased risk of MACE in patients with prior myocardial infarction.
The data presented show that the median Lp(a) concentration was 29 nmol/L among the study group. Lp(a) levels were elevated (≥ 200 nmol/L) in 1,053 patients (11.7%). There was a 29% increase in MACE risk associated with high Lp(a) concentrations in the pooled trial population (9.1% vs 7.6%; adjusted hazard ratio [adj HR] 1.29, 95% confidence intervals [CI]: 1.02–1.62; P=0.03), with a 37% increase in MI risk (6.9% vs 5.3%; adj HR 1.37, CI: 05–1.79; P=0.02). HRs for MACE with ticagrelor, compared with placebo, were 0.73 (CI: 0.48–1.11) in patients with elevated Lp(a) levels and 0.88 (CI: 0.74-1.05) in those with lower Lp(a) levels (P-interaction = 0.41). The data showed an absolute risk reduction of 2.4% and 1.2% for both groups.
Dr Patel concluded his presentation by highlighting that an Lp(a) value exceeding 200 nmol/L is associated with an increased risk of MACE in patients with prior MI. These patients may see benefits from treatment with ticagrelor in terms of absolute risk reduction. As a result of these experimental observations, insights can be gained for therapeutics evaluating the clinical potential of reducing Lp(a).
Should dual antiplatelet therapy be maintained beyond one year after a myocardial infarction?
Dual antiplatelet therapy (DAPT) consisting of aspirin and a P2Y12 inhibitor (clopidogrel, prasugrel or ticagrelor) is recommended for patients with acute coronary syndrome (ACS), for secondary prevention of cardiovascular disease (CVD). Optimal duration of DAPT requires consideration of ischaemic and bleeding risks; standard DAPT duration is 1 year, unless there are contraindications4. Myocardial infarction (MI) confers a high risk of thrombotic events; however, it is controversial to maintain DAPT beyond 1 year following MI5.
Dr Patrick Blin and his colleagues compared DAPT with single antiplatelet therapy (SAPT) with aspirin beyond 1 year after MI, in terms of the risk of MI, ischaemic stroke (IS), major bleeding (MB) and death6.
The French nationwide claims database (SNDS) was used to identify all adults hospitalised for acute MI (trigger event) with intensive care unit stay in 2013 and 2014. The study cohort consisted of patients who survived at least a year without MI or MB and had a DAPT medication possession ratio (MPR) >80%. After the index date of the study (defined as 365 days after the MI trigger event), all patients were followed for 3 years, except those who died after the index date or ceased taking aspirin after sixty days after the index date. Outcomes evaluated included: a primary composite of all-cause death, MI, IS and MB; a secondary composite of all-cause death, MI and IS; and individual outcomes. Data analysis included 3-year cumulative incidence of outcomes using Kaplan-Meier estimates or cumulative incidence function to account for death as a competing risk. The Cox proportional hazards model was used to determine associations between fatal outcomes and exposure to DAPT and SAPT. Fine and Gray models were used to assess non-fatal outcomes, which were adjusted for age, sex and exposure to specific treatments, including secondary prevention CVD medications, oral glucose-lowering medications, insulin, anticoagulants, non-steroidal anti-inflammatory drugs, corticosteroids and proton pump inhibitors.
In the absence of contraindications, standard DAPT duration of 1 year following a myocardial infarction is recommended for secondary prevention of cardiovascular disease
In total, 53,399 adults were included in the study cohort out of 105,080 admitted to intensive care units for acute MI in 2013 or 2014. Non-inclusion was most commonly attributed to death (n=12,012) and a DAPT MPR of 80% (n=25,000). At the index date, mean age was 65 years, 74.6% of those attending were men, 21.8% had diabetes, 9.4% had heart failure, 5.6% had peripheral artery disease, 72.2% had DAPT scores of 2, 61.9% had a Charlson index of 1, 79.2% had an ST-segment elevation myocardial infarction (STEMI) trigger event, and 82.6% had cardiac revascularisation (PCI 98.6%). Clopidogrel (41.5%), ticagrelor (41.1%) and prasugrel (26.2%) were among the P2Y12 inhibitors that were used at least once between the trigger event and the index date. The 3-year HR for DAPT compared with SAPT was 1.21 (CI: 1.13–1.30) for the primary composite of all-cause death, MI, IS and MB. HRs for individual outcomes were 1.16 (CI: 1.06–1.27) for death, 1.22 (CI: 1.07–1.38) for MI, 0.98 (CI: 0.80–1.20) for IS and 1.89 (CI: 1.55–2.30) for MB.
Compared with SAPT, DAPT was associated with increased risks of the primary composite outcome (21% higher, CI: 13–30), MI (22% higher, CI: 7–38), MB (89% higher, CI: 55–130) and death (16% higher, CI: 6–27). The risk of IS was similar for SAPT and DAPT. The study concluded that DAPT beyond 1 year after MI was associated with a significant risk of harm when compared with SAPT.
Takostubo syndrome during the COVID-19 pandemic
Takostubo syndrome (TTS), or stress cardiomyopathy, is a reversible cardiac condition characterised by acute ventricular dysfunction triggered by physical or emotional stress7. Activation of the sympathetic nervous system by acute stress has been suggested as a possible pathophysiological mechanism for TTS7. An increase in TTS cases was reported during the SARS-COV-19 pandemic and a recent study suggested that individuals may be more susceptible to TTS because of the psychological, mental and physical consequences of anti-pandemic measures8.
Professor Loukianos Rallidis and colleagues investigated whether TTS incidence had increased in a major tertiary hospital in Athens during the SARS-CoV-19 pandemic9. As part of the study, 316 consecutive patients with acute coronary syndrome (ACS) were admitted to the coronary care unit (CCU) of the hospital over 16 months, from March 2020 to June 2021. In order to provide a comparison with the incidence before the pandemic, 342 patients with ACS admitted to the CCU between November 2018 and February 2020 were also included in the study. Within 48 hours of admission, all patients with ACS underwent coronary angiography.
Takostubo syndrome has been reported as a cardiovascular complication of COVID-197
Patients with TTS were predominantly female (95%), with an average age of 71.1±15.4 years. The frequency of TTS was significantly higher during the pandemic (20 TTS cases among 316 ACS patients, 6.3%) than during the 16 months prior to the pandemic (9 TTS cases among 342 ACS patients, 2.6%). A comparison of the TTS cases occurring during the COVID-19 pandemic period with those occurring during the pre-pandemic period revealed an incidence rate ratio of 2.22 (95% CI: 0.97–5.54, P=0.021).
Further studies are needed to confirm whether psychological stresses associated with the SARS-COV-19 pandemic contributed to the increased incidence of TTS during the pandemic.
Patients with TTS were predominantly female (95%), with an average age of 71.1±15.4 years. The frequency of TTS was significantly higher during the pandemic (20 TTS cases among 316 ACS patients, 6.3%) than during the 16 months prior to the pandemic (9 TTS cases among 342 ACS patients, 2.6%). A comparison of the TTS cases occurring during the COVID-19 pandemic period with those occurring during the pre-pandemic period revealed an incidence rate ratio of 2.22 (95% CI: 0.97–5.54, P=0.021).
Read more on Antiplatelet therapy in ACS
References
- Boffa M, Marar T, Yeang C, Viney N, Xia S, Witztum J. et al. (2019). J Lipid Res, 60(12): 2082-2089. doi: 10.1194/jlr.p094763
- Patel S. Lipoprotein(a), cardiovascular events, and benefit of P2Y12 inhibition: insights from the PEGASUS-TIMI 54 trial. Presented at the European Society of Cardiology Congress 2022, 29 August. Barcelona. Coronary artery disease – Pharmacotherapy 3.Moderated ePosters
- Bonaca, M., Bhatt, D., Braunwald, E., Cohen, M., Steg, P., & Storey, R. et al. (2014). Am Heart J, 167(4), 437-444.e5. doi: 10.1016/j.ahj.2013.12.020
- Valgimigli M, Bueno H, Byrne RA, et al. 2017 Focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur Heart J.2018;39:213–254.
- Lev E, Ben-Assa E, et al. Dual antiplatelet therapy in patients with prior myocardial infarction. J Am Coll Cardiol Intv. 2022;15(3):294–296.
- Blin P. Should dual antiplatelet therapy be maintained beyond one year after a myocardial infarction? A cohort study within the French SNDS nationwide claims database. Presented at the European Society of Cardiology Congress 2022, 29 August. Barcelona. Acute coronary syndromes – Imaging and beyond. Moderated ePosters.
- Sharma K, Desai H, Patoliya J, Jadeja D, Gadhiya D. Takostubo syndrome a rare entity in COVID-19: a systematic review – focus on biomarkers, imaging, treatment and outcomes. SN Compr Clin Med. 2021;3(1):62-72. doi: 10.1007/s42399-021-00743-4.
- Jabri A, Kalra A, Kumar A. JAMA Netw Open. 2020; 3(7):e2014780. doi:10.1001/jamanetworkopen.2020.14780.
- Rallidis L. Takostubo syndrome during the COVID-19 pandemic: a single center experience. Presented at the European Society of Cardiology Congress 2022, 27 August. Barcelona. COVID-19 and acute coronary syndromes. Moderated ePosters.
of interest
are looking at
saved
next event
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
